Semaglutide and Diabetes Management in Thailand: A Comprehensive Look at Patient Outcomes
Diabetes is one of the most prevalent chronic diseases worldwide, and Thailand is no exception to this growing health challenge. Over the past few decades, the rates of diabetes in Thailand have steadily increased, primarily driven by factors such as changing lifestyles, poor diets, and a lack of physical activity. According to the International Diabetes Federation (IDF), approximately 4.4 million adults in Thailand are living with diabetes, and the number continues to rise.
In the context of diabetes management, semaglutide, a GLP-1 receptor agonist, has emerged as a promising treatment option, particularly for patients who struggle to achieve optimal glycaemic control through traditional therapies. This article explores the outcomes of a study involving 58 patients using Semaglutide for diabetes management, with a focus on the key data points, their implications for the Thai population, and a detailed exploration of how this medication could help tackle Thailand’s growing diabetes burden.
A Breakdown of the Data: Understanding the Key Findings
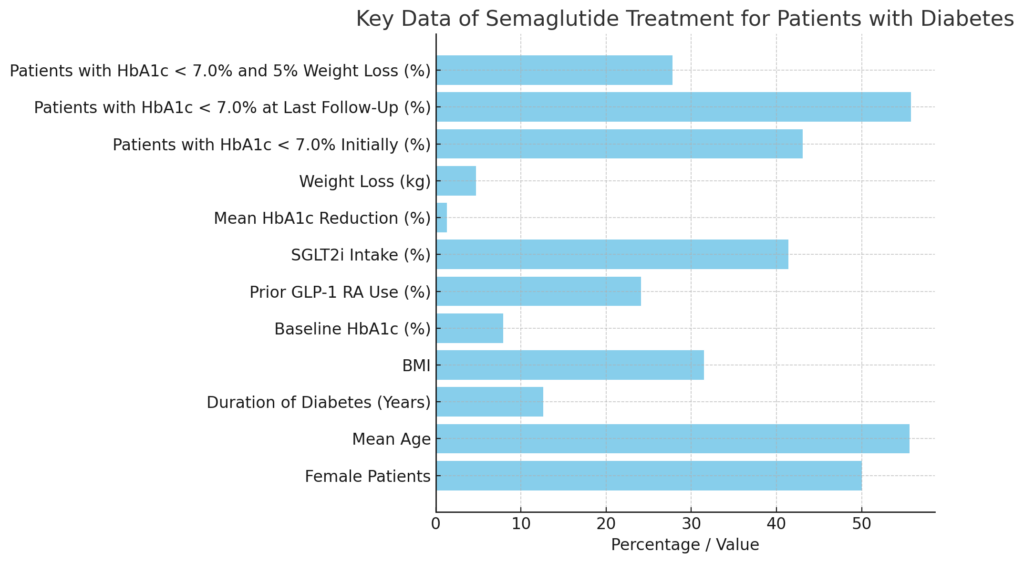
The study included 58 patients (50% female), with an average age of 55.6 years. The duration of diabetes in these patients was approximately 12.6 years, indicating that most of the patients had been living with the disease for a considerable amount of time. The average BMI was 31.5 kg/m2, which falls into the obese category, a significant factor in the development and progression of type 2 diabetes.
The following is a detailed breakdown of the data points and what they mean in diabetes management:
- Baseline HbA1c: The patients had an average baseline HbA1c of 7.9%. HbA1c is a marker of blood sugar control over time, and an HbA1c level above 7% generally indicates poor glycaemic control.
- Prior GLP-1 RA Use: Before starting Semaglutide, a significant portion of the patients (24.1%) had used GLP-1 receptor agonists, indicating that they had already experienced similar treatments.
- Concomitant SGLT2i Use: 41.4% of the patients were also taking SGLT2 inhibitors, a class of medications that helps the body eliminate excess glucose through urine.
Over a 6-month follow-up period, the study made the following observations:
- Mean HbA1c Reduction: The patients experienced a significant reduction in HbA1c levels, with a mean reduction of 1.3%, bringing many of them closer to the target HbA1c level of below 7.0%.
- Weight Loss: On average, patients lost 4.7 kg, which is a crucial factor in improving overall metabolic health, especially for those with a high BMI.
- Improvement in Glycaemic Control: By the end of the study, the proportion of patients achieving optimal glycaemic control (HbA1c < 7.0%) had increased from 43.1% to 55.8%.
- Combined Achievement of Glycaemic Control and Weight Loss: 27.8% of the patients achieved both glycaemic control and a weight loss of at least 5%, indicating comprehensive metabolic improvements.
Importantly, there were no cases of pancreatitis, cancer, or progressive retinopathy, which are potential complications associated with diabetes and its treatments.
The importance of weight loss in diabetes management
Weight plays a pivotal role in the development and progression of type 2 diabetes. In Thailand, like many other countries experiencing rapid urbanisation and lifestyle changes, obesity rates are rising. According to a report from the Thai Ministry of Public Health, the prevalence of obesity in Thailand is around 39%, and it continues to climb. Obesity is a key risk factor for the development of type 2 diabetes because excess body fat, particularly around the abdomen, leads to insulin resistance.
The mean BMI of the patients in this study was 31.5 kg/m2, classified as obese. Achieving a mean weight loss of 4.7 kg through semaglutide represents a significant achievement, as even modest weight loss can have profound effects on glycaemic control and overall health. Research has consistently shown that weight loss of 5–10% of total body weight can lead to improvements in insulin sensitivity, blood pressure, cholesterol levels, and overall cardiovascular health—all critical factors for individuals with diabetes.
For Thai patients, achieving and maintaining weight loss could help mitigate the rising rates of diabetes and obesity. However, weight loss alone is often not enough. Semaglutide’s dual role as both an appetite suppressant and a glycaemic control agent becomes crucial when combined with improvements in blood sugar control.
Glycaemic control and long-term health outcomes
The HbA1c level is one of the most important metrics in diabetes management, as it reflects a patient’s average blood sugar levels over the past two to three months. In Thailand, many patients struggle to reach the recommended target of HbA1c < 7%, which is crucial for reducing the risk of complications such as neuropathy, nephropathy, retinopathy, and cardiovascular disease.
In this study, 43.1% of patients had HbA1c levels below 7.0% at baseline, but by the end of the study, this increased to 55.8%. This improvement is significant, as even small reductions in HbA1c can lead to better long-term outcomes. Research has shown that for every 1% reduction in HbA1c, there is a 21% reduction in the risk of diabetes-related death and a 14% reduction in the risk of heart attack.
Moreover, achieving glycaemic control is particularly important for Thai patients, who may face a higher risk of complications due to the lack of widespread access to healthcare in rural areas. For these individuals, reducing their HbA1c levels with a medication like semaglutide can be life-changing.
The impact of semaglutide on women’s health in Thailand is significant.
Interestingly, the study had an equal distribution of male and female patients (50% female), making it valuable to explore how semaglutide may specifically benefit women with diabetes. In Thailand, diabetes affects both men and women, but women face unique challenges due to hormonal fluctuations, pregnancy, and menopause, which can complicate blood sugar control.
Gestational diabetes, a form of diabetes that occurs during pregnancy, is particularly prevalent in Thailand. Women who develop gestational diabetes are at a higher risk of developing type 2 diabetes later in life. Moreover, women with diabetes are more prone to cardiovascular complications, and they are less likely to achieve glycaemic control compared to men. Thus, a medication like Semaglutide, which addresses both weight and glycaemic control, is an invaluable tool for improving health outcomes in women.
The weight loss aspect of semaglutide is especially relevant for Thai women, as obesity rates are on the rise among females, driven by cultural and lifestyle changes. For women managing diabetes, achieving a healthy weight can have significant benefits for reproductive health, reducing the risk of complications during pregnancy and lowering the chances of developing other obesity-related conditions.
The Role of Semaglutide in Thailand’s Healthcare Landscape
Thailand’s healthcare system is well-developed, with universal healthcare provided through the Universal Coverage Scheme (UCS). However, like many countries, the Thai healthcare system faces challenges in managing the rising rates of non-communicable diseases such as diabetes. According to the World Health Organisation (WHO), diabetes has become one of the leading causes of death in Thailand, underscoring the need for more effective treatments and management strategies.
Semaglutide, with its dual ability to improve glycaemic control and promote weight loss, is well-suited to address these challenges. However, access to innovative medications like Semaglutide may still be limited for certain populations, particularly those living in rural areas or low-income groups. Ensuring that medications like Semaglutide are accessible to all segments of the population could have a transformative impact on diabetes outcomes in Thailand.
Furthermore, Thailand’s rising rates of sedentary lifestyles, increased consumption of processed foods, and urbanisation all contribute to the diabetes epidemic. The Thai government has already initiated public health campaigns to encourage healthier eating and more physical activity, but medications like semaglutide can provide an additional tool for those who need more targeted interventions to manage their diabetes and weight.
Long-Term Outlook: Preventing Diabetes Complications
Diabetes is a progressive disease, and without proper management, it can lead to severe complications such as heart disease, stroke, kidney failure, and blindness. The patients in this study experienced significant improvements in their glycaemic control and weight, which are both critical factors in preventing these long-term complications.
One of the most encouraging aspects of this study is that there were no cases of pancreatitis, cancer, or progressive retinopathy reported among the patients, which are potential risks associated with poor diabetes management. This highlights the safety profile of Semaglutide, especially over a 6-month follow-up period.
In Thailand, where rural areas may limit access to specialised diabetes care, medications like semaglutide can significantly improve the quality of life for diabetes patients by reducing the risk of complications. Education on how to maintain long-term glycaemic control and prevent complications should be a key component of diabetes care in the country.
Our Conclusion: The promise of semaglutide for Thailand’s diabetes epidemic persists.
The results of this study clearly demonstrate the effectiveness of semaglutide in promoting significant weight loss and improving glycaemic control, two critical factors in managing diabetes. Semaglutide offers a promising solution for Thailand, where diabetes rates are rising and complications are becoming more common. Its ability to address the dual issues of weight management and blood sugar regulation makes it an ideal treatment option for patients struggling with type 2 diabetes, particularly those dealing with obesity and insulin resistance.
Given the rising prevalence of obesity and diabetes in Thailand, incorporating medications like Semaglutide into the healthcare system could greatly enhance the management of these conditions. Along with public health initiatives focussing on lifestyle changes, increasing access to medications like semaglutide could play a crucial role in controlling Thailand’s diabetes epidemic.
Ultimately, semaglutide’s role in improving both metabolic health and reducing diabetes complications is significant. For patients and healthcare providers alike, understanding how to effectively maintain the progress made during semaglutide treatment will be key to ensuring long-term health benefits. This comprehensive approach—combining medication, lifestyle changes, and preventative care—offers the best path forward for individuals struggling with diabetes in Thailand and beyond.

Leave a Reply